Dr. Paresh Bang | Matruchhaya Spine Clinic
Meet Our Doctor
Dr. Paresh Bang
Consultant Spine Surgeon

Surgery for Tuberculosis spine In Bhandara
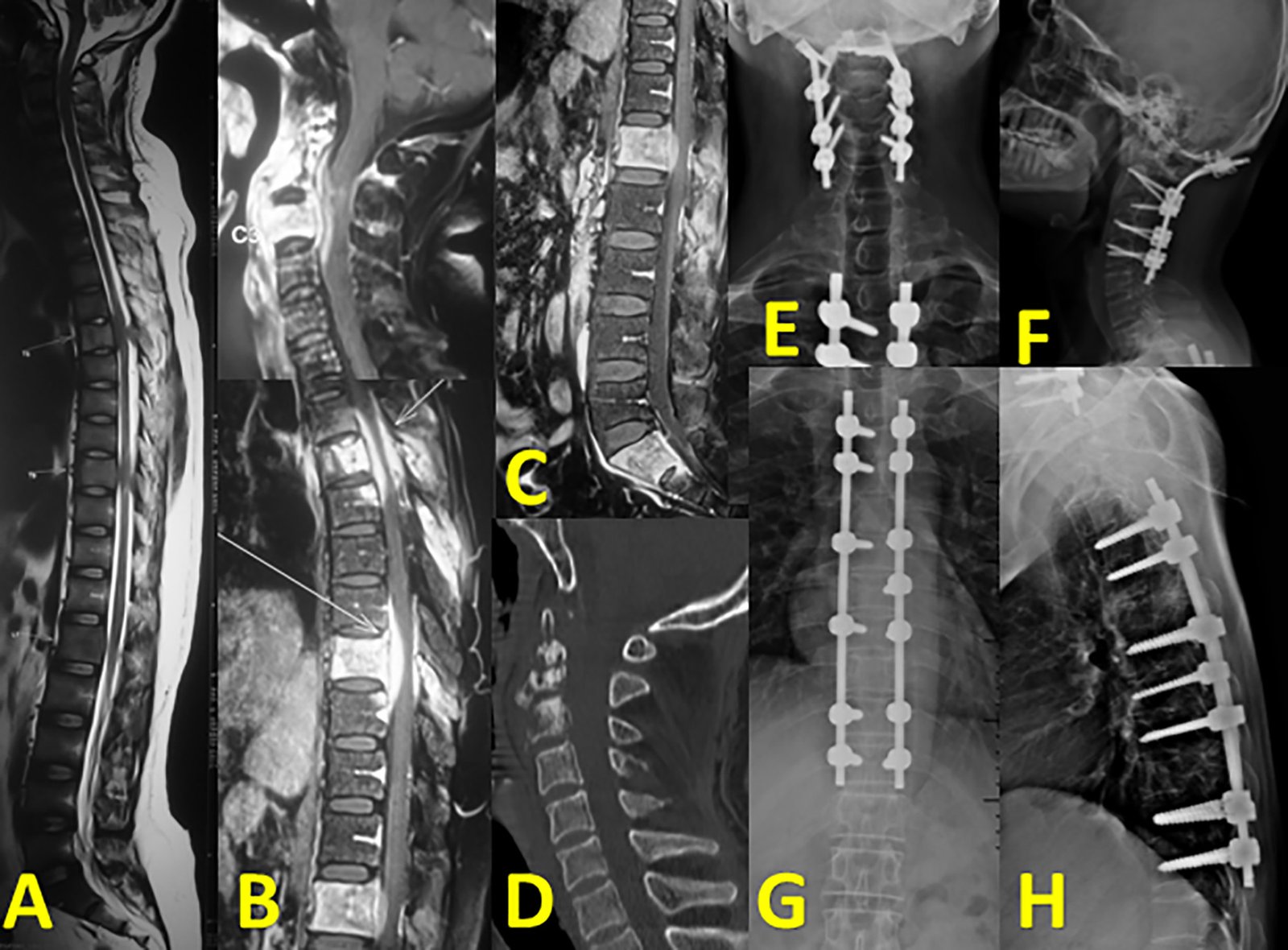
Surgery for Tuberculosis spine
Surgery for TB of the spine, also referred to as Pott’s disease or spinal TB, is generally indicated in complications or when medical therapy alone is not sufficient. Nevertheless, more than 95% of patients with spinal TB respond well to anti-tuberculosis drugs, whereas sometimes surgery may be necessary.
When Surgery is Indicated for Spinal Tuberculosis:
1.Neurological Deficits:
Major surgery is usually justified due to gradual or rapid deterioration of neurological function as a consequence of spinal cord or nerve root compression by abscesses, granulation tissue, or bone fragments. Failure of medical treatment with resultant loss of impact on the spinal cord necessitates surgical decompression
2. Spinal Instability:
Advanced spinal TB leads to destruction of the vertebral bodies, which may cause instability or deformity, such as kyphosis. Pain is severe and may lead to functional impairment; surgical stabilization with instrumentation, such as rods or screws, may be required for restoration of stability.
3. Severe Kyphosis or Deformity:
If there is any important deformity of the spine, especially in younger patients, surgical intervention for reversal of the deformity may be needed to prevent late-onset disability or complications such as difficulty in breathing.
4. Draining the Abscess:
Surgery may be necessary if the paravertebral abscess or cold abscess is quite large and is not responding to medical care, where this abscess and infected tissue are drained and removed.
5. Failure of Inpatient Management:
If anti-tuberculosis therapy (ATT) is ineffective after an adequate period, or if there is evidence of disease progression, surgery may be needed to control the infection.
Types of Surgery for Spinal Tuberculosis:
- Decompression Surgery:
- Indication: When the spinal cord or nerve roots are compressed due to abscesses, bone fragments, or inflamed tissues, causing neurological symptoms like weakness or paralysis.
- Procedure: Involves removing the infected and damaged tissue, including parts of the vertebrae or disc, to relieve pressure on the spinal cord or nerves.
- Laminectomy: Removal of the lamina (part of the vertebra) to decompress the spinal cord.
- Corpectomy: Removal of one or more vertebral bodies to decompress the spinal cord and remove infected tissue.
- Spinal Fusion and Stabilization:
- Indication: If the TB infection has caused spinal instability due to the destruction of vertebral bodies, fusion surgery may be required to stabilize the spine.
- Procedure: Involves fusing the affected vertebrae together using bone grafts (taken from the patient or donor) and stabilizing the spine with metal rods, screws, or plates. This prevents further deformity and helps maintain the integrity of the spine.
- Anterior Spinal Fusion: The spine is accessed from the front of the body to remove the infected tissue and fuse the vertebrae.
- Posterior Spinal Fusion: The spine is accessed from the back to stabilize the affected vertebrae.
- Combined Approach: In severe cases, both anterior and posterior approaches are used for maximum stability.
- Abscess Drainage:
- Indication: When large abscesses (pus-filled collections) form due to the infection, causing pressure on surrounding tissues and potentially the spinal cord.
- Procedure: Abscesses may be drained through open surgery or minimally invasive techniques to relieve pressure and remove the infected material.
- Kyphoplasty or Vertebroplasty:
- Indication: In cases where TB has caused vertebral collapse but the deformity is mild, these minimally invasive procedures can help stabilize the spine.
- Procedure:
- Vertebroplasty: Bone cement is injected into the collapsed vertebra to stabilize it.
- Kyphoplasty: A balloon is first inserted and inflated to restore some height to the collapsed vertebra before cement is injected to stabilize it.
what happen after Surgery for Spinal Tuberculosis:
After spinal TB surgery, the recovery process can vary based on the severity of the disease, the extent of the surgery, and the patient’s overall health. Here’s what typically happens after surgery for spinal tuberculosis (Pott’s disease):
1. Immediate Post-Operative Care:
Hospital Stay: the patient may spend several days in the hospital. Pain management, monitoring for any complications, and ensuring stability are the primary focuses.
Pain Control: is crucial immediately after surgery. Medications, including analgesics and anti-inflammatory drugs, are given to manage post-surgical pain.
Wound Care: Surgical wounds are closely monitored for signs of infection. The area is kept clean and sterile to prevent post-operative infections.
Antibiotic Therapy (ATT): Even after surgery, anti-tuberculosis therapy (ATT) will continue for several months (usually 6 to 12 months) to fully eradicate the TB infection from the body.
2. Monitoring for Complications:
Neurological Function: Monitoring of neurological functions is essential, especially if the surgery was done to relieve spinal cord compression. Improvement in sensation and motor function is observed over time.
Infection and Healing: The surgical site is monitored for any signs of infection or poor wound healing, and imaging tests may be done to track the progress of recovery.
Spinal Stability: In cases where spinal stabilization devices (such as rods or screws) were used, follow-up imaging (X-rays, CT scans, or MRIs)
3. Rehabilitation:
Physical Therapy: Once the patient has recovered from the acute effects of surgery, a physical therapy program is initiated. This program focuses on:
Strengthening the back and core muscles.
Improving mobility and flexibility.
Preventing further deformities or complications.
Helping the patient regain functional independence.
Mobility Aids: Depending on the severity of the disease and surgery, patients may need temporary use of mobility aids, such as braces or walkers, during the rehabilitation period.
4. Continued Anti-Tuberculosis Treatment (ATT):
Even after surgery, the patient will continue taking anti-tuberculosis medications (typically a combination of drugs like isoniazid, rifampicin, pyrazinamide, and ethambutol) for a prolonged period. It ensures the complete eradication of infection.
Adherence to this medication regimen is essential to prevent recurrence or drug resistance.
5. Recovery Timeline:
Short-Term Recovery: The immediate post-surgical recovery period typically takes a few weeks to months, depending on the complexity of the surgery. During this period, activities will be restricted, and follow-up appointments will be frequent.
Long-Term Recovery: including spinal stability and neurological recovery, can take several months to year. In cases of severe neurological involvement or deformity, recovery may take longer, and some neurological deficits may be permanent.
Return to Activities: The ability to resume normal activities will depend on the extent of the disease and surgery. Some patients may return to light activities in a few weeks, while others may need several months of rehabilitation before they can resume daily tasks or work.
6. Potential Complications Post-Surgery:
Infection: at the surgical site due to the underlying TB infection.
Neurological Complications: Though surgery aims to relieve compression on the spinal cord, there’s a risk of residual or new neurological issues, including numbness, weakness, or even paralysis.
Spinal Deformity: If kyphosis (spinal curvature) was not fully corrected during surgery, or if the spine continues to collapse, further deformities may develop over time.
Hardware Complications: In cases where spinal instrumentation was used, there is a small risk of hardware failure or complications, such as loosening or breaking of rods/screws.
Non-Union or Delayed Healing: If spinal fusion was performed, the bone graft may take time to heal, and in some cases, it may not fully fuse, requiring further surgery.
7. Prognosis:
Improvement in Neurological Symptoms: If surgery was done to decompress the spinal cord, there is often significant improvement in neurological symptoms (such as weakness, numbness, or paralysis). However, extent of recovery depends on how long spinal cord was compressed the severity of damage before surgery.
Reduction in Pain and Stability: Spinal stabilization surgeries typically result in a significant reduction in pain and improvement in spinal stability.
Preventing Long-Term Complications: If surgery is successful and combined with ongoing ATT, most patients can achieve a good long-term prognosis with minimal risk of recurrence or permanent disability.
Preoperative and Postoperative Management:
- Preoperative Management:
- Anti-Tuberculous Medications (ATT): Even if surgery is needed, the cornerstone of TB treatment is still anti-tuberculous drug therapy. Patients will typically be on a regimen of multiple drugs (e.g., isoniazid, rifampicin, ethambutol, and pyrazinamide) for at least 6-9 months or longer. Surgery is considered only when these medications fail to control the disease or when urgent decompression or stabilization is required.
- Infection Control: Preoperative imaging (MRI, CT scans) and lab tests will help the surgeon assess the extent of infection and the involvement of the spinal cord or nerves.
- Postoperative Care:
- Continued ATT: After surgery, anti-tuberculous medications must be continued to ensure the infection is fully eradicated.
- Physical Therapy: Early mobilization and rehabilitation are important to help patients recover strength and maintain mobility after surgery.
- Regular Monitoring: Follow-up imaging and clinical assessments are necessary to monitor for recurrence of infection and complications.
Risks and Complications of Surgery for Spinal Tuberculosis:
As with any major surgery, there are potential risks and complications, including:
- Infection: Both surgical site infections and worsening of TB infection if not controlled effectively.
- Neurological Damage: Though surgery aims to relieve nerve compression, there is a risk of nerve or spinal cord injury.
- Spinal Instability: If fusion does not heal properly, or if the hardware fails, there can be ongoing spinal instability.
- Recurrence of TB: Despite surgery and medication, TB can recur, particularly in immunocompromised patients.
- Kyphotic Deformity: If not corrected adequately during surgery, patients may develop or worsen kyphosis (hunchback) after the operation.Contact Us
Conclusion:
Surgery for spinal tuberculosis is often lifesaving or critical to preventing severe deformity, neurological damage, or ongoing infection. It is typically performed in combination with anti-tuberculous drug therapy and may involve decompression, spinal fusion, abscess drainage, or stabilization of the spine. Given the complex nature of spinal TB, it’s important for patients to be treated by an experienced spine surgeon with expertise in both infectious diseases and complex spinal surgery.Visit Our Hospital
