Dr. Paresh Bang | Matruchhaya Spine Clinic
Meet Our Doctor
Dr. Paresh Bang
Consultant Spine Surgeon

Surgery for Tuberculosis spine In Yavatmal
Surgery for Tuberculosis spine
When Surgery is Indicated for Spinal Tuberculosis:
Surgery for spinal tuberculosis is typically considered when:
- Neurological Deficits: Compression of the spinal cord or nerve roots due to abscesses, bone fragments, or deformity, leading to symptoms such as weakness, numbness, or paralysis.
- Severe Spinal Deformity: Significant kyphosis (hunchback) or other deformities caused by the collapse of the vertebrae.
- Spinal Instability: When the vertebral bodies are significantly damaged by the TB infection, causing instability and risk of collapse.
- Persistent Pain or Progressive Disease: Despite medical treatment, the disease progresses or pain becomes intolerable.
- Abscesses: Large abscesses (pus-filled cavities) that do not resolve with medical therapy and need to be drained surgically.
- Failure of Conservative Treatment: When medical management with anti-tuberculous drugs does not control the disease adequately.
Types of Surgery for Spinal Tuberculosis:
- Decompression Surgery:
- Indication: When the spinal cord or nerve roots are compressed due to abscesses, bone fragments, or inflamed tissues, causing neurological symptoms like weakness or paralysis.
- Procedure: Involves removing the infected and damaged tissue, including parts of the vertebrae or disc, to relieve pressure on the spinal cord or nerves.
- Laminectomy: Removal of the lamina (part of the vertebra) to decompress the spinal cord.
- Corpectomy: Removal of one or more vertebral bodies to decompress the spinal cord and remove infected tissue.
- Spinal Fusion and Stabilization:
- Indication: If the TB infection has caused spinal instability due to the destruction of vertebral bodies, fusion surgery may be required to stabilize the spine.
- Procedure: Involves fusing the affected vertebrae together using bone grafts (taken from the patient or donor) and stabilizing the spine with metal rods, screws, or plates. This prevents further deformity and helps maintain the integrity of the spine.
- Anterior Spinal Fusion: The spine is accessed from the front of the body to remove the infected tissue and fuse the vertebrae.
- Posterior Spinal Fusion: The spine is accessed from the back to stabilize the affected vertebrae.
- Combined Approach: In severe cases, both anterior and posterior approaches are used for maximum stability.
- Abscess Drainage:
- Indication: When large abscesses (pus-filled collections) form due to the infection, causing pressure on surrounding tissues and potentially the spinal cord.
- Procedure: Abscesses may be drained through open surgery or minimally invasive techniques to relieve pressure and remove the infected material.
- Kyphoplasty or Vertebroplasty:
- Indication: In cases where TB has caused vertebral collapse but the deformity is mild, these minimally invasive procedures can help stabilize the spine.
- Procedure:
- Vertebroplasty: Bone cement is injected into the collapsed vertebra to stabilize it.
- Kyphoplasty: A balloon is first inserted and inflated to restore some height to the collapsed vertebra before cement is injected to stabilize it.
Preoperative and Postoperative Management:
- Preoperative Management:
- Anti-Tuberculous Medications (ATT): Even if surgery is needed, the cornerstone of TB treatment is still anti-tuberculous drug therapy. Patients will typically be on a regimen of multiple drugs (e.g., isoniazid, rifampicin, ethambutol, and pyrazinamide) for at least 6-9 months or longer. Surgery is considered only when these medications fail to control the disease or when urgent decompression or stabilization is required.
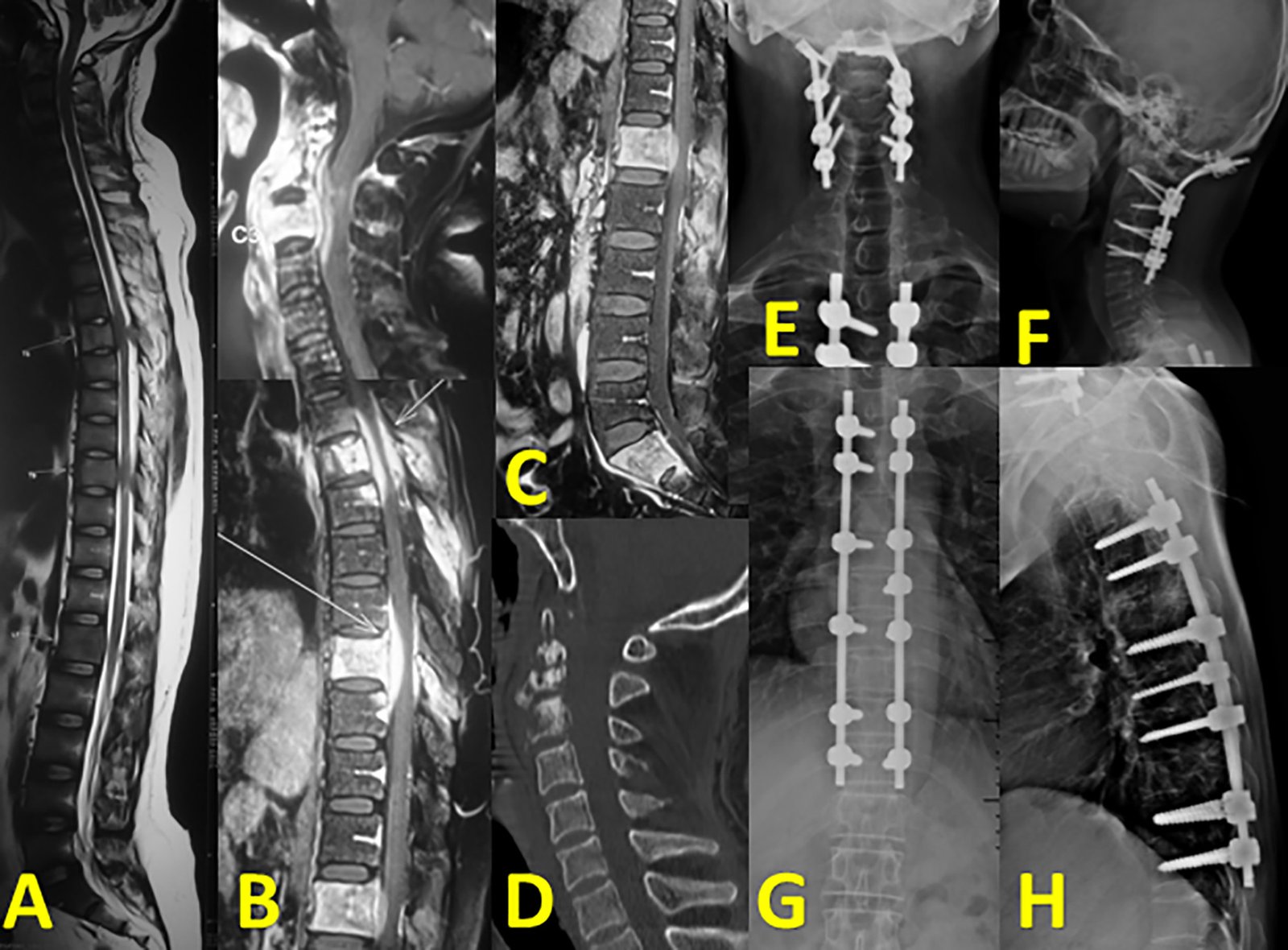
- Infection Control: Preoperative imaging (MRI, CT scans) and lab tests will help the surgeon assess the extent of infection and the involvement of the spinal cord or nerves.
- Postoperative Care:
- Continued ATT: After surgery, anti-tuberculous medications must be continued to ensure the infection is fully eradicated.
- Physical Therapy: Early mobilization and rehabilitation are important to help patients recover strength and maintain mobility after surgery.
- Regular Monitoring: Follow-up imaging and clinical assessments are necessary to monitor for recurrence of infection and complications.
Risks and Complications of Surgery for Spinal Tuberculosis:
As with any major surgery, there are potential risks and complications, including:
- Infection: Both surgical site infections and worsening of TB infection if not controlled effectively.
- Neurological Damage: Though surgery aims to relieve nerve compression, there is a risk of nerve or spinal cord injury.
- Spinal Instability: If fusion does not heal properly, or if the hardware fails, there can be ongoing spinal instability.
- Recurrence of TB: Despite surgery and medication, TB can recur, particularly in immunocompromised patients.
- Kyphotic Deformity: If not corrected adequately during surgery, patients may develop or worsen kyphosis (hunchback) after the operation.
Recovery After Surgery for Spinal Tuberculosis:
Recovery can vary depending on the extent of the surgery and the severity of the disease, but in general:
- Hospital Stay: Patients may stay in the hospital for 1-2 weeks, depending on their condition.
- Physical Rehabilitation: Physiotherapy starts early and may continue for several months to regain strength or mobility.
- Bracing: In some cases, patients may need to wear a brace to support the spine during healing.
- Long-Term Follow-Up: Regular check-ups with the surgeon and infectious disease specialist are crucial to monitor healing, check for recurrence, and manage any complications.Contact Us
Conclusion:
Surgery for spinal tuberculosis is often lifesaving or critical to preventing severe deformity, neurological damage, or ongoing infection. It is typically performed in combination with anti-tuberculous drug therapy and may involve decompression, spinal fusion, abscess drainage, or stabilization of the spine. Given the complex nature of spinal TB, it’s important for patients to be treated by an experienced spine surgeon with expertise in both infectious diseases and complex spinal surgery.Visit Our Hospital
